Breast Cancer Interventional Oncology
Breast Cancer Interventional Oncology
Breast Cancer
Interventional Oncology
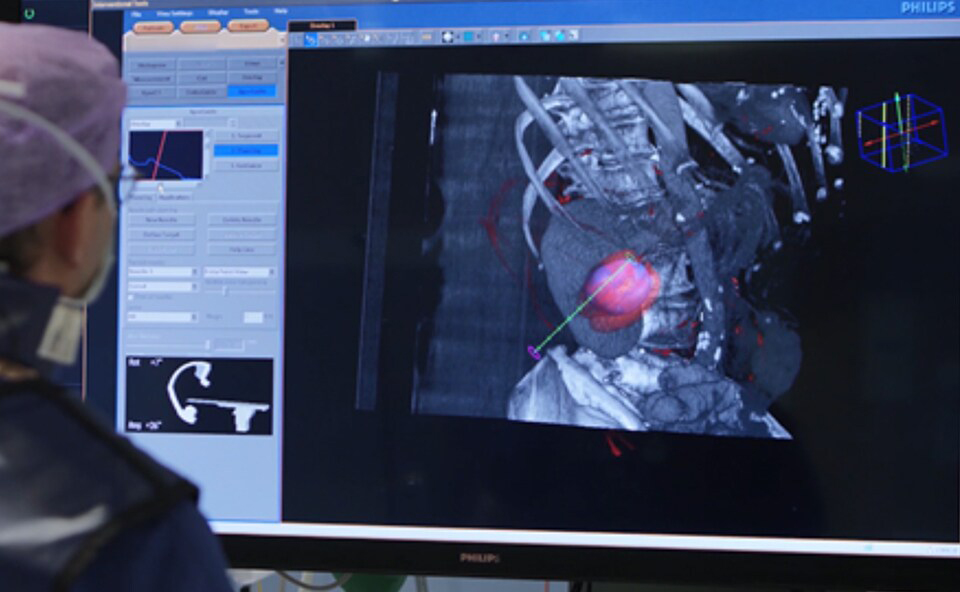
Interventional oncology consists of image guided procedures which directly treat solid tumors. Minimally invasive methods such as radiofrequency ablation (RFA), microwave ablation (MWA), cryoablation, high intensity focused ultrasound (HIFU), and laser ablation have been used to treat breast cancer as an alternative to surgery in some instances. Ablation therapy uses heat or cold administered directly to the tumor via the use of specialized probes to remove malignant tissue. Imaging is used to guide the probes into the proper position and track the effectiveness of the treatment.
Studies have supported the use of ablation for patients with very early-stage (tumor size ≤ 2 cm) breast cancer who are elderly, in poor physical condition, or who want good cosmetic results. Ablation has also been studied when used in combination with surgery for breast cancer. While ablation procedures have the potential to reduce complications, improve cosmesis, and shorten hospital stays, there are still challenges associated with utilizing these minimally invasive methods including the optimization of anesthesia, imaging of the tumor, and ensuring complete histological ablation with clean margins.
Percutaneous ablative techniques include both thermal and non-thermal approaches. Thermal approaches include heat-based procedures (radiofrequency, microwave ablation and ultrasound) and cold-based procedures (cryoablation). Irreversible electroporation is a non-thermal ablative approach. These are described in more detail below.
- Radiofrequency ablation (RFA) – is a minimally invasive procedure that uses electrical energy and heat to destroy cancer cells. A needle is inserted through the skin into the cancer tissue and the heat produces coagulation necrosis and subsequent cell death. While RFA is a simple, repeatable, standardized, lower risk procedure, it is limited by only having a small area of effectiveness since electrical impedance develops as the tissue boils and becomes charred.4 This insulates the tissue from the electrical signal and results in an effective area of only few millimeters. Besides tumor location, other factors which impact the effectiveness of RFA include the size and number of tumors and the need for a large tumor-free margin. While RFA is not typically used as a first-line treatment for breast cancer, it may be considered in certain cases, particularly for small tumors or as part of a multidisciplinary treatment approach. It is more commonly used for the treatment of benign breast tumors, such as fibroadenomas.
- Microwave ablation (MWA) – MWA uses high frequency microwave energy to heat and kill cancer cells. A thin probe containing an antenna which emits microwaves is into the tumor. The probe produces intense heat that destroys tumor tissue via coagulation necrosis, often within 10 minutes. In the context of breast cancer, MWA is a minimally invasive technique that has been investigated as a potential treatment option, particularly for small tumors. MWA is not commonly used as a primary treatment for breast cancer, but it has been explored in clinical studies and research settings.
- Cryoablation – Cryoablation or cryosurgery that uses extreme cold to destroy tumors. The procedure causes rapid cooling of the target tissue, resulting in intracellular ice crystal formation that destroys organelle and cell membranes and induces membrane pore formation that disrupts the electrochemical gradient. Cellular tonicity is also disturbed, causing lethal transmembrane fluid shifts. If these changes do not cause immediate cell death, they often initiate apoptosis. The ability to visualize ice ball formation, the edge of which marks the 0°C isotherm, in cryoablation on several imaging modalities is a particular benefit. Cryotablation’s role in the treatment of breast cancer has not been established.
- High-Intensity Focused Ultrasound (HIFU) – HIFU is a non-invasive therapeutic technique that uses ultrasound waves to treat various medical conditions, including breast cancer. In the context of breast cancer treatment, HIFU is sometimes used as a focal therapy to target and destroy cancerous tissue without the need for surgery. HIFU works by focusing high-intensity ultrasound waves on a specific target within the body. The focused ultrasound energy generates heat, causing thermal ablation (destruction) of the targeted tissue.
During a HIFU procedure for breast cancer, the patient is positioned such that the ultrasound waves can be accurately targeted at the tumor. Real-time imaging, such as ultrasound or MRI, is often used to guide the HIFU treatment and monitor its progress.
The role of ablation procedures in the treatment of breast cancer
- Advantages of ablation vs. surgery – less invasive than traditional surgical procedures with the ability to be performed sometimes on an outpatient basis. These procedures are typically associated with minimal side effects compared to traditional treatments like surgery or radiation and have a shorter recovery time.
- Limitations of ablation vs. surgery – ablative approaches are only suitable for treating small tumors that are well-defined and accessible. The effectiveness of the procedures can vary, and they may not be suitable for all types and stages of breast cancer. Most ablative approaches are still considered investigational for breast cancer treatment with its used primarily as a part of clinical trials or under certain circumstances where other treatments are not viable options. They are not considered a standard or first-line treatment for breast cancer in many medical guidelines.
References
- Carriero S, Lanza C, Pellegrino G, et al. Ablative therapies for breast cancer: State of Art. Technol Cancer Res Treat. 2023;22:15330338231157193. doi: 10.1177/15330338231157193.
- Peek MCL, Ahmed M, Napoli A, et al. Minimally invasive ablative techniques in the treatment of breast cancer: a systematic review and meta-analysis. Int J Hyperthermia. 2017;33:191-202. doi: 10.1080/02656736.2016.1230232.
- Peek MC, Ahmed M, Napoli A, ten Haken B, McWilliams S, Usiskin SI, Pinder SE, van Hemelrijck M, Douek M. Systematic review of high-intensity focused ultrasound ablation in the treatment of breast cancer. Br J Surg. 2015;102:873-82. doi: 10.1002/bjs.9793. PMID: 26095255.
- Zulkifli D, Manan HA, Yahya N, Hamid HA. The Applications of High-Intensity Focused Ultrasound (HIFU) Ablative Therapy in the Treatment of Primary Breast Cancer: A Systematic Review. Diagnostics (Basel). 2023;13:2595. doi: 10.3390/diagnostics13152595.
- Dai Y, Liang P, Yu J. Percutaneous Management of Breast Cancer: a Systematic Review. Curr Oncol Rep. 2022;24:1443-1459. doi: 10.1007/s11912-022-01290-4.
- van de Voort EMF, Struik GM, Birnie E, Moelker A, Verhoef C, Klem TMAL. Thermal Ablation as an Alternative for Surgical Resection of Small (≤ 2 cm) Breast Cancers: A Meta-Analysis. Clin Breast Cancer. 2021;21:e715-e730. doi: 10.1016/j.clbc.2021.03.004.
- Mauri G, Sconfienza LM, Pescatori LC, Fedeli MP, Alì M, Di Leo G, Sardanelli F. Technical success, technique efficacy and complications of minimally-invasive imaging-guided percutaneous ablation procedures of breast cancer: A systematic review and meta-analysis. Eur Radiol. 2017;27:3199-3210. doi: 10.1007/s00330-016-4668-9.