Pancreatic Cancer
Pancreatic Cancer
Multidisciplinary Discussion on Pancreas Cancer
Listen as doctors from multiple disciplines discuss treatment options for patients with pancreatic cancer.
INTRODUCTION
Pancreatic cancer
Types of Pancreatic Cancer
There are several types of pancreatic cancer which are typically divided into one of two types being either an exocrine tumor or an endocrine tumor based on the different cell types within the pancreas which are associated with cancer.
Exocrine Tumors – The exocrine part of the pancreas produces digestive enzymes that play a crucial role in the digestion of food. These digestive enzymes are released into the small intestine to help break down complex nutrients into smaller, absorbable components. Pancreatic exocrine malignancies are by far the most prevalent form pancreatic cancer. This includes:
- Pancreatic adenocarcinoma: adenocarcinomas account for approximately 95% of exocrine pancreas cancers. These tumors typically begin in the pancreatic ducts. They are called acinar cell carcinomas when they arise from the cells that produce the pancreatic enzymes, which occurs less frequently.
- Ampullary cancer: these tumors originate in the ampulla of Vater, the location where the pancreatic and bile ducts converge and drain into the small intestine. While not specifically a pancreatic tumor, its treatment is similar to the other pancreatic exocrime tumors.
- Other less frequent types of exocrine carcinoma: includes adenosquamous carcinomas, squamous cell carcinomas, signet ring cell carcinomas, undifferentiated carcinomas, and undifferentiated carcinomas with giant cells. Ampullary cancer, also known as carcinoma of the ampulla of Vater, originates in the ampulla of Vater, the location where the pancreatic and bile ducts converge and drain into the small intestine. Although they aren’t quite pancreatic tumors, auxiliary malignancies are included here as their treatments are similar.
Endocrine Tumors (Islet Cell or Neuroendocrine Tumors) – The pancreas produces a variety of hormones, including insulin, which regulate the functions of specific body organs or cells. Islet cells, also known as islet of Langerhans, are clusters of cells within the pancreas that play a crucial role in regulating blood sugar (glucose) levels in the body. Pancreatic endocrine tumors, also known as pancreatic neuroendocrine tumors (PNETs) or islet cell tumors, are a group of rare tumors that arise from the hormone-producing cells (islet cells) in the pancreas. These tumors can be classified based on the specific type of hormone-producing cells involved.
Main types of pancreatic endocrine tumors include:
- Insulinomas: tumors that arise from the beta cells of the islets of Langerhans and produce excessive amounts of insulin. This leads to hypoglycemia (low blood sugar), which can cause symptoms such as confusion, dizziness, and fainting.
- Glucagonomas: tumors originating from the alpha cells of the islets, glucagonomas produce excess glucagon. Elevated levels of glucagon can result in hyperglycemia (high blood sugar), skin rashes (necrolytic migratory erythema), weight loss, and diarrhea.
- Gastrinomas: tumors which are associated with a condition called Zollinger-Ellison syndrome. These tumors produce excess gastrin, leading to increased stomach acid production. Symptoms may include peptic ulcers, abdominal pain, and diarrhea.
- VIPomas (Vasoactive Intestinal Peptide-producing tumors): these tumors produce vasoactive intestinal peptide (VIP), leading to a condition known as VIPoma syndrome. Symptoms include severe diarrhea, dehydration, and electrolyte imbalances.
- PPomas (Pancreatic Polypeptide-producing tumors): these tumors produce excessive pancreatic polypeptide, and they are often non-functioning, meaning they do not cause specific hormonal symptoms. However, they can cause abdominal pain or be discovered incidentally.
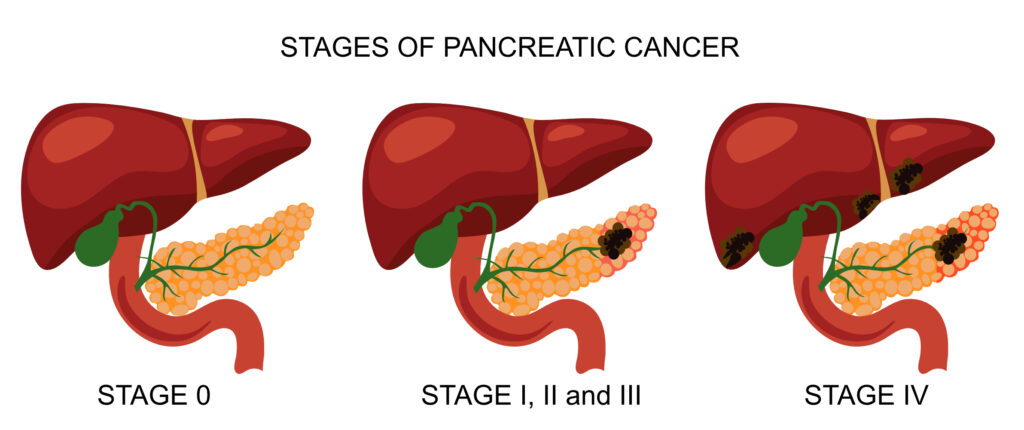
Staging
The most important predictor of survival from pancreatic cancer is stage of the cancer at diagnosis with localized cancer having a better survival. Pancreatic cancer can occur in five stages, denoted by the letters 0, I, II, III, and IV. The greater the number, the greater the extent of cancer spread. The stage of pancreatic cancer is also described by the “TNM” system. The TNM staging is a system used to classify the extent of cancer based on the size of the primary tumor (T), the involvement of nearby lymph nodes (N), and the presence of distant metastasis (M).
T (Primary Tumor):
- TX: Primary tumor cannot be assessed.
- T0: No evidence of primary tumor.
- Tis: Carcinoma in situ (early cancer that has not invaded nearby tissues).
- T1: Tumor limited to the pancreas, measuring 2 cm (or less) in greatest dimension.
- T2: Tumor limited to the pancreas, measuring more than 2 cm in greatest dimension.
- T3: Tumor extends beyond the pancreas but without involvement of major blood vessels.
- T4: Tumor involves major blood vessels.
N (Regional Lymph Nodes):
- NX: Regional lymph nodes cannot be assessed.
- N0: No regional lymph node metastasis.
- N1: Regional lymph node metastasis.
T (Primary Tumor):
- MX: Distant metastasis cannot be assessed.
- M0: No distant metastasis.
- M1: Distant metastasis present.
M (Distant Metastasis):
- MX: Distant metastasis cannot be assessed.
- M0: No distant metastasis.
- M1: Distant metastasis present.
The stages of pancreatic cancer include:
Stage 0 (Tis, N0, M0):
- Tis: Carcinoma in situ (early cancer that has not invaded nearby tissues).
- No regional lymph node involvement (N0).
- No distant metastasis (M0).
Stage I (T1, N0, M0):
- T1: Tumor limited to the pancreas, measuring 2 cm (or less) in greatest dimension.
- No regional lymph node involvement (N0).
- No distant metastasis (M0).
Stage II (T2, N0, M0):
- T2: Tumor limited to the pancreas, measuring more than 2 cm in greatest dimension.
- No regional lymph node involvement (N0).
- No distant metastasis (M0).
Stage III (T3, N1, M0):
- T3: Tumor extends beyond the pancreas but without involvement of major blood vessels.
- Regional lymph node involvement (N1).
- No distant metastasis (M0).
Stage IV (Any T, Any N, M1):
- Any T: Tumor of any size.
- Any N: May or may not involve regional lymph nodes.
- M1: Distant metastasis is present.
Stage IV is the most advanced stage, indicating that the cancer has spread to other organs or distant lymph nodes. Pancreatic cancer is often diagnosed at later stages, and treatment options and prognosis depend on the specific characteristics of the cancer at the time of diagnosis.
Risk Factors
Several risk factors are associated with an increased likelihood of developing pancreatic cancer. It’s important to note that having one or more risk factors does not guarantee the development of pancreatic cancer, and many people diagnosed with pancreatic cancer do not have identifiable risk factors. However, understanding these risk factors can help in identifying individuals who may be at higher risk. Common risk factors for pancreatic cancer include:
Age
pancreatic cancer is more common in older adults, with the majority of cases diagnosed in individuals over the age of 65.
Tobacco Use
cigarette smoking is a significant risk factor for pancreatic cancer. Smokers are more likely to develop pancreatic cancer than non-smokers, and the risk increases with the number of years of smoking.
Family History
individuals with a family history of pancreatic cancer, particularly in first-degree relatives (parents, siblings, children), have an increased risk. Certain genetic syndromes, such as hereditary pancreatitis and familial atypical multiple mole melanoma (FAMMM) syndrome, are also associated with a higher risk.
Inherited Genetic Mutations
specific genetic mutations, such as those in the BRCA2, BRCA1, PALB2, CDKN2A, and ATM genes, can increase the risk of pancreatic cancer. Genetic counseling may be recommended for individuals with a family history of pancreatic cancer or known genetic mutations.
Chronic Pancreatitis
long-term inflammation of the pancreas is associated with an increased risk of pancreatic cancer.
Diabetes
people with long-standing diabetes, especially those diagnosed with diabetes later in life, may have an elevated risk of pancreatic cancer.
Obesity
obesity has been identified as a potential risk factor for pancreatic cancer.
Dietary Factors
a diet high in red and processed meats, as well as low fruit and vegetable intake, may contribute to an increased risk of pancreatic cancer.
Occupational Exposures
certain occupational exposures, such as to certain chemicals, may be associated with an increased risk of pancreatic cancer.
Treatment:
Treatment options for pancreas cancer depend on various factors, including the type and stage of the cancer, the presence of hormone receptors, the patient’s overall health, and individual preferences. Common treatments include surgery, chemotherapy, radiation, and/or interventional procedures.
Detailed information on each of these options can be found in the modules listed below.
References
- Cancer Facts & Figures 2023, American Cancer Society (ACS), Atlanta, Georgia, 2023.
- SEER*Explorer: An interactive website for SEER cancer statistics [Internet]. Surveillance Research Program, National Cancer Institute. [Cited 2023 December 28].
- National Comprehensive Cancer Network®. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Pancreatic Adenocarcinoma. Version 1.2024 — December 13, 2023.