Liver Radiation
Liver Radiation
Liver
Radiation
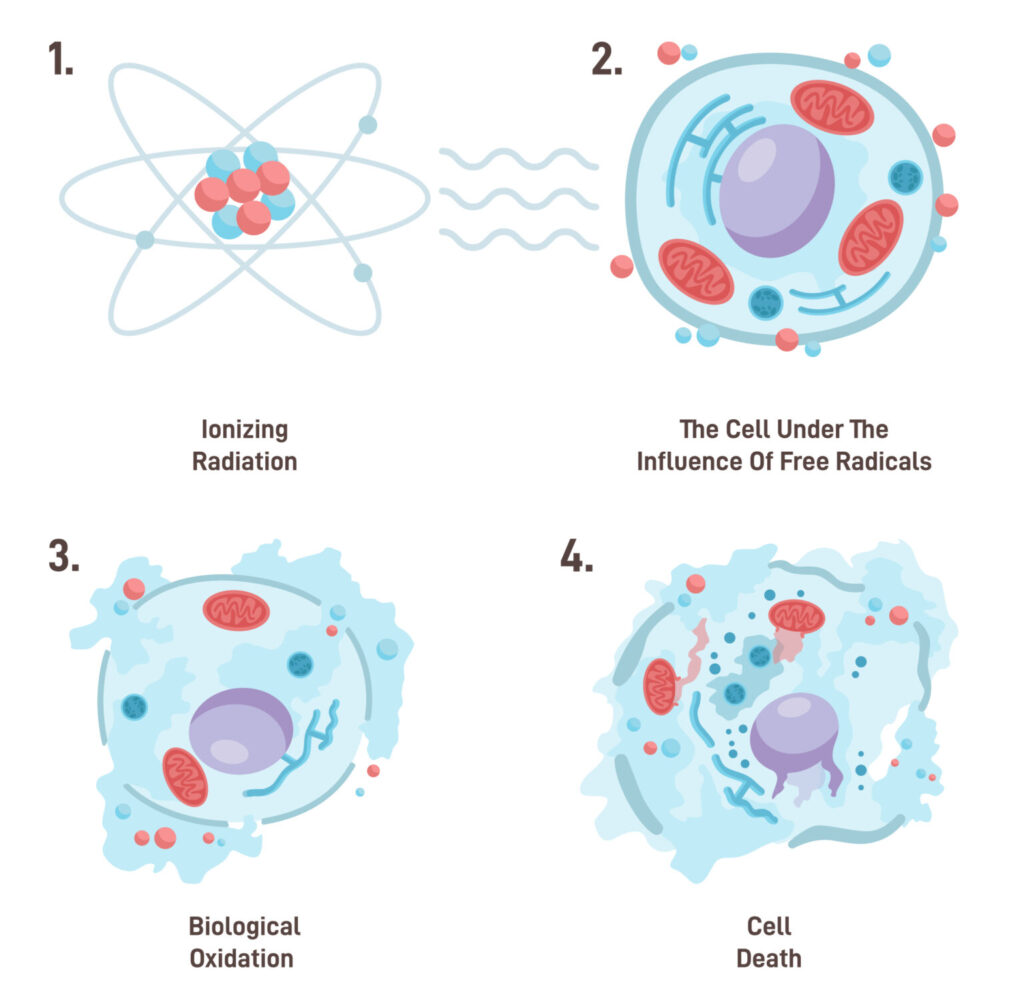
Radiation therapy is one of the treatment options for liver cancer, particularly for patients who are not candidates for surgery or other local treatments. The goal of radiation therapy is to destroy cancer cells while minimizing damage to surrounding healthy tissue.
Radiation therapy involves the use of high-energy X-rays or other particles to target and destroy cancer cells or inhibit their ability to grow and divide. The decision to include radiation in the treatment plan for pancreatic cancer depends on several factors, including the type and stage of the cancer, the characteristics of the tumor, the type of surgery performed, and individual patient considerations.
The goal of radiation therapy is to target and destroy cancer cells or slow down their growth. It can be administered in different ways, and the choice of radiation therapy depends on the specific characteristics of the cancer and the overall treatment plan. Radiation therapy can be utilized alone or in combination with other localized treatment approaches.
External Beam Radiation – this is the most common type of radiation therapy for breast cancer. It involves delivering radiation from outside the body to the targeted area. There are different types of external beam radiation techniques used for liver cancer treatment, each with its own advantages and considerations. Main types:
- Stereotactic Body Radiation Therapy (SBRT) – is a specialized form of external beam radiation therapy that delivers highly focused, high-dose radiation to the tumor in a few treatment sessions. It is used to treat used for small tumors or when surgery is not an option. While SBRT provides higher local tumor control rates, it requires advanced tumor tracking, image guidance, and respiratory management to minimize the risk of morbidity.1,2 Several studies have confirmed the clinical utility of SBRT for the treatment of HCC with most of the studies for early-stage liver cancer.3 A large meta-analysis reported 87% local control at 1 year and 80% overall 1 year survival associated with the use of SBRT for liver cancer.4 SBRT has also been studied as a bridge to liver transplantation in early-stage inoperable HCC.5
- Intensity-Modulated Radiation Therapy (IMRT) – allows the radiation dose to conform more precisely to the shape of the tumor by modulating the intensity of the radiation beams. This enables better dose distribution and reduces the dose of radiation to critical structures in or near the liver. Studies have reported local control rates of 70% and 47% at 1 and 3 year respectively for IMRT and overall 1 and 3 year survival rates of 59% and 33%.6,7
- Proton beam therapy (PBT) – an advanced form of radiation therapy that uses protons rather than X-rays to treat cancer. It is particularly beneficial for treating hepatocellular carcinoma (HCC). Protons are accelerated to high speeds using a cyclotron or synchrotron and the energy of the proton beam is controlled precisely to target the tumor at a specific depth. The protons release their maximum energy directly at the tumor site, minimizing damage to surrounding healthy tissues. PBT allows for precise targeting of the liver tumor, sparing healthy liver tissue and nearby organs. Due to its precision, PBT reduces the risk of side effects compared to traditional radiation therapy. Studies have shown that PBT can be effective in controlling local tumor growth and potentially improving survival rates with local control rates of 80% to 95% and an overall survival rate of 60% at 2 years.8,9
Indications for radiation therapy for liver cancer:
- Unresectable Tumors: When the tumor cannot be surgically removed due to size, location, or the patient’s overall health.
- Bridge to Transplant: To control tumor growth in patients awaiting liver transplantation.
- Palliation: To relieve symptoms such as pain caused by the tumor pressing on other organs or structures.
References
- Guckenberger M, Sweeney RA, Wilbert J, Krieger T, Richter A, Baier K, et al. Image-guided radiotherapy for liver cancer using respiratory-correlated computed tomography and cone-beam computed tomography. Int J Radiat Oncol Biol Phys. 2008;71:297–304. doi: 10.1016/j.ijrobp.2008.01.005
- Kubo HD, Hill BC. Respiration gated radiotherapy treatment: a technical study. Phys Med Biol. 1996;41:83–91.
- Chen CP. Role of Radiotherapy in the Treatment of Hepatocellular Carcinoma. J Clin Transl Hepatol. 2019 Jun 28;7(2):183-190. doi: 10.14218/JCTH.2018.00060
- Qi WX, Fu S, Zhang Q, Guo XM. Charged particle therapy versus photon therapy for patients with hepatocellular carcinoma: a systematic review and meta-analysis. Radiother Oncol. 2015;114:289–295. doi: 10.1016/j.radonc.2014.11.033
- Moore A, Cohen-Naftaly M, Tobar A, Kundel Y, Benjaminov O, Braun M, et al. Stereotactic body radiation therapy (SBRT) for definitive treatment and as a bridge to liver transplantation in early stage inoperable hepatocellular carcinoma. Radiat Oncol. 2017;12:163. doi: 10.1186/s13014-017-0899-4
- Hou JZ, Zeng ZC, Wang BL, Yang P, Zhang JY, Mo HF. High dose radiotherapy with image-guided hypo-IMRT for hepatocellular carcinoma with portal vein and/or inferior vena cava tumor thrombi is more feasible and efficacious than conventional 3D-CRT. Jpn J Clin Oncol. 2016;46:357–362. doi: 10.1093/jjco/hyv205
- Yoon HI, Lee IJ, Han KH, Seong J. Improved oncologic outcomes with image-guided intensity-modulated radiation therapy using helical tomotherapy in locally advanced hepatocellular carcinoma. J Cancer Res Clin Oncol. 2014;140:1595–1605. doi: 10.1007/s00432-014-1697-0
- Hong TS, Wo JY, Yeap BY, Ben-Josef E, McDonnell EI, Blaszkowsky LS, et al. Multi-Institutional Phase II Study of High-Dose Hypofractionated Proton Beam Therapy in Patients With Localized, Unresectable Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma. J Clin Oncol. 2016 Feb 10;34(5):460-8. doi: 10.1200/JCO.2015.64.2710
- Chadha AS, Gunther JR, Hsieh CE, Aliru M, Mahadevan LS, Venkatesulu BP, Crane CH, et al. Proton beam therapy outcomes for localized unresectable hepatocellular carcinoma. Radiother Oncol. 2019 Apr;133:54-61. doi: 10.1016/j.radonc.2018.10.041