Breast Cancer
Breast Cancer
Multidisciplinary Discussion on Breast Cancer
Listen as doctors from multiple disciplines discuss treatment options for patients with breast cancer.
Breast Cancer
Introduction
Breast cancer is a type of cancer that begins in the cells of the breast. It can occur in both men and women, but it is far more common in women. Although the precise etiology of breast cancer is unknown, a number of risk factors have been found, including genetic abnormalities (mutations in BRCA1 and BRCA2), age, gender, family history, hormones, and specific lifestyle variables.
Breast cancer is the most frequently diagnosed cancer and the fourth leading cause of cancer death in the United States with the majority of cases (99%) occurring in women (1). In 2023, an estimated 300,000 individuals were diagnosed with breast cancer in the United States with approximately 1 in 8 women (13%) diagnosed with invasive breast cancer in their lifetime.(2)(3) Approximately 44,000 patients previously diagnosed with breast cancer died of the disease in 2023.(2) The overall 5-year relative survival rate for breast cancer is 90.8% (4) with survival rates varying by how far the cancer has spread including a 99% 5-year survival rate for non-invasive localized breast cancer, 86% for regional cancer, and 30% for distant breast cancer.(5)
Breast cancers are classified based on several key factors:
Location of Origin
Most breast cancers are adenocarcinomas, beginning in glandular tissue. Cancer can start in the lobules (milk-producing glands) or ducts (tubes that carry milk to the nipple).
In situ vs. invasive
In situ cancers remain within the ducts or lobules (such as ductal carcinoma in situ (DCIS)), while invasive cancers spread beyond these areas (including invasive ductal carcinoma (IDC), invasive lobular carcinoma (ILC) or mixed invasive carcinoma).
Cell differentiation
Cancer cells can be well-differentiated (more normal-looking cells, slower-growing), moderately differentiated or poorly differentiated (more abnormal/lack of normal features, grow and spread faster), which indicates how aggressive the cancer is.
Biology and receptors
Some cancers have hormone receptors (estrogen or progesterone) or overexpression of human epidermal growth factor 2 (HER2), which provides insight into what fuels cancer growth, guiding treatment options with targeted therapies.
This classification helps determine the most effective treatment approach.
Molecular Testing
Breast cancer is further classified by molecular characteristics that are associated with clinical presentation, response to therapy, and prognosis. Hormone receptor positive (HR+) cancers are those that test positive for estrogen receptors (ER) or progesterone receptors (PR), or both. HER2+ cancers are those which test positive for the HER2 protein (3).
- HR+/HER2: Comprising about 68% of cases, this is the most prevalent molecular subtype of breast cancer. It responds well to hormone therapy and tends to grow more slowly, being less aggressive compared to other subtypes.
- HR+/HER2+: This subtype is characterized by being positive for both hormone receptors and HER2. It accounts for approximately 10% of breast cancer cases and is associated with worse outcomes due to its aggressive nature. It often requires both hormone therapy and HER2-targeted treatments.
- HER2+ (HR-): Representing around 15-20% of cases, this subtype tests positive for HER2 but negative for hormone receptors. It tends to be more aggressive, with a higher likelihood of recurrence, and has improved prognosis due to advances in targeted therapies.
- Triple-Negative Breast Cancer (TNBC): This subtype tests negative for all three biomarkers (ER, PR, HER2), making up about 10-15% of all breast cancer cases. TNBC is generally more aggressive and has a higher chance of spreading and recurring. It is more common in younger women, particularly those under 40, and in African American women.
- HER2-low: This subtype may be either HR positive or negative but exhibits low levels of HER2 expression. It represents a newer classification and may benefit from targeted therapies despite its lower HER2 expression.
Staging
The most important predictor of survival from breast cancer is stage of the cancer at diagnosis with localized cancer having a better survival Breast cancer can occur in five stages, denoted by the letters 0, I, II, III, and IV. The greater the number, the greater the extent of cancer spread. The stage of breast cancer is also described by the “TNM” system:
- T: Tumor size (in centimeters)
- N: Number of near by lymph nodes with cancer
- M: Whether the cancer has metastasized or spread to other organs of the body (0 = no spread, 1 = it has spread)
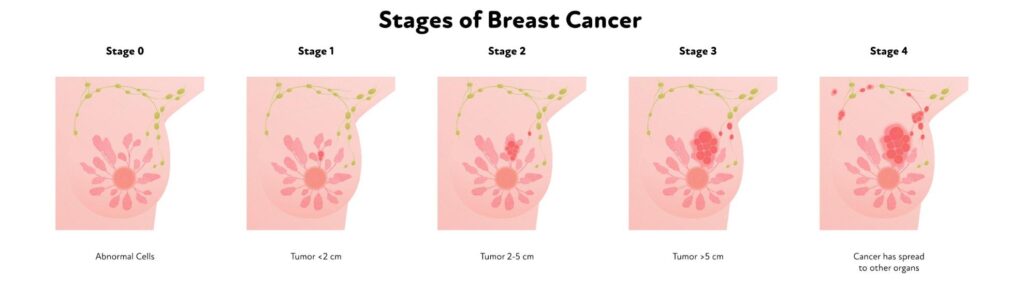
The stages of breast cancer include (7)(8):
Stage 0: The disease is only in the ducts and lobules of the breast. It has not spread to the surrounding tissue. It is also called noninvasive cancer (Tis, N0, M0).
Stage I: The disease is invasive. Cancer cells are now in normal breast tissue. There are 2 types:
- Stage IA: The tumor is up to 2 centimeters (cm). It has not spread to the lymph nodes (T1, N0, M0).
- Stage IB: The tumor is in the breast and is less than 2 cm and is present in 1-3 axillary lymph nodes. Or the tumor is present in 1-3 axillary lymph nodes of the breast and there is no tumor in the breast tissue.
Stage II: There are 2 types of Stage II breast cancer, all of which are considered invasive.
- Stage IIA: The tumor may be of any size and has spread to 4-9 lymph nodes. Or the tumor is larger than 5 cm and has spread to 1-3 lymph nodes. It has not spread to other parts of the body.
- Stage IIB: The tumor is 2 to 5 cm and the disease has spread to 1 to 3 axillary lymph nodes or the tumor is larger than 5 cm but has not spread to the axillary lymph nodes.
Stage III: There are 2 types of Stage III breast cancer, all of which are considered invasive.
- Stage IIIA: The tumor may be of any size and has spread to 4-9 lymph nodes. Or the tumor is larger than 5 cm and has spread to 1-3 lymph nodes. It has not spread to other parts of the body.
- Stage IIIB: The tumor may be any size and the disease has spread to the chest wall or skin and may be in up to 9 lymph nodes. It may cause swelling of the breast.Inflammatory breast cancer is considered Stage IIIB.
- Stage IIIC: There may be no sign of cancer in the breast, or a tumor may be any size and may have spread to the chest wall or breast skin. The disease has spread to 10 or more axillary lymph nodes, or nodes above or below the collarbone or next to the sternum.
Stage IV: Metastatic breast cancer. The tumor can be any size and the disease has spread to other organs and tissues, such as the bones, lungs, brain, liver, distant lymph nodes, or chest wall (any T, any N, M1).
Risk Factors
Several risk factors are associated with an increased likelihood of developing breast cancer. It’s important to note that having one or more risk factors does not guarantee the development of breast cancer, and many people diagnosed with breast cancer have no identifiable risk factors. Conversely, individuals without apparent risk factors can still develop the disease. Here are some common risk factors for breast cancer:
Gender and Age – Being female is the primary risk factor for breast cancer. Women are much more likely to develop breast cancer than men. The risk increases with age, and the majority of breast cancer cases occur in women over the age of 55.
Family History and Genetics – A family history of breast cancer, especially in first-degree relatives (mother, sister, daughter), increases the risk.
Genetic mutations – Inherited gene mutations, such as BRCA1 and BRCA2, significantly elevate the risk of breast cancer and ovarian cancer.
Personal History of Breast Cancer or Certain Non-Cancerous Diseases – Women who have had breast cancer in one breast have an increased risk of developing cancer in the other breast. Certain non-cancerous breast diseases, such as atypical hyperplasia, can increase the risk.
Reproductive Factors – Early onset of menstruation (before age 12) and late menopause (after age 55) are associated with an increased risk. The increased risk may be due to longer lifetime exposure to estrogen and progesterone hormones. Delayed childbirth or never having children can contribute to a higher risk. Early age at first childbirth and breastfeeding for a longer duration may have a protective effect.
Radiation Exposure – Previous radiation therapy to the chest area, especially during adolescence or young adulthood, can elevate the risk.
Lifestyle Factors
Alcohol consumption – Regular and excessive alcohol intake is linked to an increased risk of breast cancer.
Physical inactivity – Regular physical activity may lower breast cancer risk, particularly in postmenopausal women. Even a few hours a week can be beneficial, with more activity offering greater protection.
Not having children or not breastfeeding – Women who have not had children or had their first child after age 30 have a slightly higher breast cancer risk, while having multiple pregnancies at a younger age lowers risk. However, breast cancer risk increases for the first decade after childbirth before decreasing over time. Breastfeeding may also slightly reduce breast cancer risk, particularly if done for a year or more, possibly due to fewer lifetime menstrual cycles.
Hormone Replacement Therapy (HRT) – Long-term use of combined hormone replacement therapy (estrogen and progesterone) after menopause can increase the risk of breast cancer.
Click here for more detailed information on risk factors associated with the development of breast cancer.
Treatment
Treatment options for breast cancer depend on various factors, including the type and stage of the cancer, the presence of hormone receptors, the patient’s overall health, and individual preferences. Common treatments include surgery, chemotherapy, hormone therapy, targeted therapy, radiation, and/or interventional procedures4 Detailed information on each of these options can be found in the modules listed below.
The goals of breast cancer treatment are tailored to the individual characteristics of the cancer and patient preferences. Generally, the primary objectives of breast cancer treatment include:
- Cure or Long-Term Remission – the primary goal is to eliminate the cancer from the body and achieve a cure whenever possible. For some patients, particularly those with early-stage breast cancer, curative treatment may involve surgery, radiation therapy, and/or systemic therapies like chemotherapy, hormone therapy, or targeted therapy.
- Local Control – preventing the recurrence of cancer in the breast or the nearby lymph nodes is a critical aspect of treatment. Surgical procedures, such as lumpectomy or mastectomy, combined with radiation therapy, aim to achieve local control.
- Prevention of Metastasis – adjuvant systemic therapies (chemotherapy, hormone therapy, targeted therapy) are often used to target and eliminate any cancer cells that may have traveled from the primary tumor to other locations.
- Symptom Management – alleviating symptoms associated with the disease, such as pain, fatigue, and discomfort, is an important part of breast cancer care.
- Palliative Care may be incorporated to improve the quality of life, especially in advanced or metastatic breast cancer.
- Preservation of Breast and Body Image – balancing the need for effective cancer treatment with preserving the patient’s physical appearance and emotional well-being is crucial. Breast-conserving surgery (lumpectomy) is an option when possible, and breast reconstruction may be considered after mastectomy.
- Maintaining or Improving Quality of Life – minimizing the impact of treatment on the patient’s overall quality of life is an important consideration. Supportive care, including psychological and emotional support, is often integrated into the treatment plan.
References
- Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2024;74(1):12-49.
- Cancer Facts & Figures 2023, American Cancer Society (ACS), Atlanta, Georgia, 2023.
- https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf [Cited 2024 Oktober 9].
- SEER*Explorer: An interactive website for SEER cancer statistics [Internet]. Surveillance Research Program, National Cancer Institute. [Cited 2023 December 28].
- https://www.cancer.org/cancer/types/breast-cancer/understanding-a-breast-cancer-diagnosis/breast-cancer-survival-rates.html
- https://www.cancer.org/cancer/types/breast-cancer/understanding-a-breast-cancer-diagnosis/breast-cancer-hormone-receptor-status.html [Cited 2024 October 9].
- https://www.facs.org/for-patients/the-day-of-your-surgery/breast-cancer-surgery/breast-cancer-types/breast-cancer-staging/ [Cited 2024 October 9].
- https://www.cancer.org/cancer/types/breast-cancer/understanding-a-breast-cancer-diagnosis/stages-of-breast-cancer.html [Cited 2024 October 9].
- https://www.cancer.org/cancer/types/breast-cancer/risk-and-prevention/breast-cancer-risk-factors-you-cannot-change.html [Cited 2024 October 10].
- https://www.lbbc.org/about-breast-cancer/what-is-breast-cancer
- National Comprehensive Cancer Network®. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Breast Cancer. Version 5.2023 — December 5, 2023.