CRC Interventional Oncology
CRC Interventional Oncology
Colorectal
Interventional Oncology
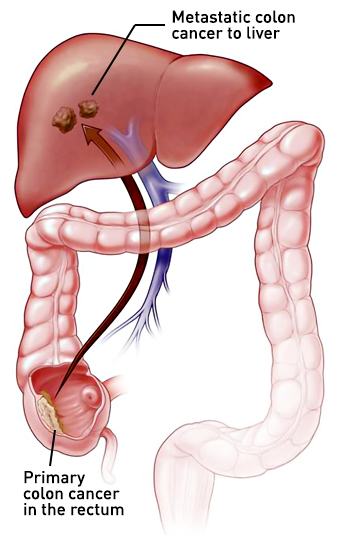
Interventional oncology consists of image guided procedures which directly treat solid tumors. These procedures are typically performed in patients whose colorectal cancer has metastasized to the liver. Approximately 20% to 34% of patients will have metastatic colorectal cancer when diagnosed and 50% to 60% of patients diagnosed with non-metastatic disease will develop colorectal metastases over time.1 Metastatic disease most often develops more than 6 months after local or regional treatment with the liver being the most common site.
Interventional image-guided procedures provide minimally invasive alternatives for select patients with a few small metastases in accessible locations.2 Potential interventional oncology procedures include both percutaneous and transarterial endovascular approaches which are used in the following settings:
Neoadjuvant setting (prior to surgery) – treatment for unresectable tumors in patients with limited metastatic tumor burden or used to reduce the size of tumors to make them potentially resectable by surgery.
Adjuvant setting (following surgical resection of a tumor) – used in combination with chemotherapy to destroy any remnant tumor in select patients.
Salvage setting – for patients who have not been able to achieve successful treatment following chemotherapy.
Surgical resection of colorectal liver metastases remains the preferred treatment option as a result of better outcomes compared to interventional ablative approaches with the potential exception of small metastases.3 Minimally invasive interventional oncology procedures are often used to treat tumors which cannot be resected by surgery or for tumors in patients who are poor candidates for surgery due to medical issues.
resected by surgery or for tumors in patients who are poor candidates for surgery due to medical issues.
Interventional Oncology Procedures for Metastatic Colorectal Cancer
Percutaneous ablative procedures
Percutaneous ablative techniques include both thermal and non-thermal approaches. Thermal approaches include heat-based procedure (radiofrequency and microwave ablation) and cold-based procedures (cryoablation). Thermal ablative techniques have been shown to be effective in the local treatment of tumors and are associated with a low recurrence rate. Irreversible electroporation is currently the only non-thermal ablative approach. These are described in more detail below.
- Radiofrequency ablation (RFA) – is a minimally invasive procedure that uses electrical energy and heat to destroy cancer cells.
 A needle is inserted through the skin into the cancer tissue and the heat produces coagulation necrosis and subsequent cell death. While RFA is a simple, repeatable, standardized, lower risk procedure, it is limited by only having a small area of effectiveness since electrical impedance develops as the tissue boils and becomes charred.4 This insulates the tissue from the electrical signal and results in an effective area of only few millimeters. The effectiveness of RFA is also reduced when used near large blood vessels since this results in a heat sink effect where the heat is dissipated by the blood flowing through these vessels. Besides tumor location, other factors which impact the effectiveness of RFA include the size and number of tumors and the need for a large tumor-free margin.
A needle is inserted through the skin into the cancer tissue and the heat produces coagulation necrosis and subsequent cell death. While RFA is a simple, repeatable, standardized, lower risk procedure, it is limited by only having a small area of effectiveness since electrical impedance develops as the tissue boils and becomes charred.4 This insulates the tissue from the electrical signal and results in an effective area of only few millimeters. The effectiveness of RFA is also reduced when used near large blood vessels since this results in a heat sink effect where the heat is dissipated by the blood flowing through these vessels. Besides tumor location, other factors which impact the effectiveness of RFA include the size and number of tumors and the need for a large tumor-free margin. - Microwave ablation – Microwave ablation uses high frequency microwave energy to heat and kill cancer cells. A thin probe containing an antenna which emits microwaves is into the tumor. The probe produces intense heat that destroys tumor tissue via coagulation necrosis, often within 10 minutes. Microwave ablation has a number of advantages over RFA including faster heating over a larger area, shorter procedure time, no need for a grounding pad, resistance to the heat sink effect, and less pain.
- Cryoablation – Cryoablation
causes rapid cooling of the target tissue, resulting in intracellular ice crystal formation that destroys organelle and cell membranes and induces membrane pore formation that disrupts the electrochemical gradient. Cellular tonicity is also disturbed, causing lethal transmembrane fluid shifts. If these changes do not cause immediate cell death, they often initiate apoptosis. The ability to visualize ice ball formation, the edge of which marks the 0°C isotherm, in cryoablation on several imaging modalities is a particular benefit.
- Irreversible electroporation (IRE) therapy –
IRE is a nonthermal ablation technique that induces cell death by disrupting the electric potential gradient across cell membranes, leading to the formation of permanent nanopores through the plasma membrane, altering cellular transport and ultimately cell homeostasis.5 The procedure involves the delivery of a series of high voltage direct current electrical pulses between two electrodes placed within a target area surrounding the tumor. Since IRE is a nonthermal treatment, it has the advantage over thermal ablative treatments since the treatment zone can cross large blood vessels and bile ducts without damaging these vital structures.
Endovascular transarterial procedures
While ablation and resection are potentially curative options for metastatic CRC, only around 20% of patients are eligible for these treatments. Endovascular transarterial approaches provide an alternative treatment option for patients who are not candidates for surgical or percutaneous ablative procedures. Endovascular transarterial treatments use a minimally invasive approach and use image-guidance to deliver therapy into small hepatic arteries that provide the blood supply to the tumor in the liver. These procedures are performed in patients with metastatic CRC who are not candidates for surgical or percutaneous ablative procedures or for patients who are not responsive to therapy, have disease progression or toxicity to systemic chemotherapy. While these procedures are not curative, they can improve survival and improve quality of life.
Examples of endovascular transarterial procedures include:
- Transarterial embolization (TAE) – TAE involves the placement of tiny particles made of gelatin beads or sponges into the small arteries of the liver and blocking the blood flow to the tumor. The beads are delivering through a catheter inserted through the femoral artery and guided to the liver.
The therapy provides a local tumor treatment which does not block the blood supply to healthy liver tissue.
- Transarterial chemoembolization (TACE) – TACE is similar procedure to TAE but also involves the local delivery of chemotherapy to the tumor while the blood supply is blocked. This reduces the risk of systemic side effects associated with chemotherapy and the drug remains for a longer period of time since the arteries remain blocked.
- Drug-eluting bead transarterial chemoembolization (DEB-TACE) – DEB-TACE uses microspheres to precisely release local chemotherapy over time to the tumor. The beads are “loaded” with drugs and the therapy is delivered directly to the tumor, substantially reducing the concentration of the drug in the systemic circulation and decreasing the risk of side effects.
- Transarterial radioembolization (Yttrium 90 or Y90) – Y90 combines radiation therapy with embolization. Microscopic glass or resin microspheres are loaded with the radioisotope yttrium-90 (90Y) and injected into the hepatic artery. This enables the local delivery of radiation to the tumor, avoiding the complications associated systemic or local/regional radiation therapy. While the primary goal of Y90 therapy is to slow tumor growth and reduce cancer symptoms, it has also been used to reduce the size of tumors to permit enable surgical resection.
References
- Qaderi SM, Galjart B, Verhoef C, Slooter GD, Koopman M, Verhoeven RHA, de Wilt JHW, van Erning FN. Disease recurrence after colorectal cancer surgery in the modern era: a population-based study. Int J Colorectal Dis. 2021 Nov;36(11):2399-2410. doi: 10.1007/s00384-021-03914-w.
- Hickey R, Vouche M, Sze DY, et al. Cancer concepts and principles: primer for the interventional oncologist-part II. J Vasc Interv Radiol. 2013;24(8):1167-1188. doi:10.1016/j.jvir.2013.04.023
- Wang LJ, Zhang ZY, Yan XL, Yang W, Yan K, Xing BC. Radiofrequency ablation versus resection for technically resectable colorectal liver metastasis: a propensity score analysis. World J Surg Oncol 2018;16(1):207.
- Tsitskari M, Filippiadis D, Kostantos C, et al. The role of interventional oncology in the treatment of colorectal cancer liver metastases. Ann Gastroenterol. 2019;32(2):147-155. doi:10.20524/aog.2018.0338.
- Xiao D, Yao C, Liu H, Li C, Cheng J, Guo F, Tang L. Irreversible electroporation and apoptosis in human liver cancer cells induced by nanosecond electric pulses. Bioelectromagnetics. 2013 Oct;34(7):512-20. doi: 10.1002/bem.21796. Epub 2013 Jun 6. PMID: 23740887.
- Narayanan G, Bhatia S, Echenique A, Suthar R, Barbery K, Yrizarry J. Vessel patency post irreversible electroporation. Cardiovasc Intervent Radiol. 2014 Dec;37(6):1523-9. doi: 10.1007/s00270-014-0988-9.

 causes rapid cooling of the target tissue, resulting in intracellular ice crystal formation that destroys organelle and cell membranes and induces membrane pore formation that disrupts the electrochemical gradient. Cellular tonicity is also disturbed, causing lethal transmembrane fluid shifts. If these changes do not cause immediate cell death, they often initiate apoptosis. The ability to visualize ice ball formation, the edge of which marks the 0°C isotherm, in cryoablation on several imaging modalities is a particular benefit.
causes rapid cooling of the target tissue, resulting in intracellular ice crystal formation that destroys organelle and cell membranes and induces membrane pore formation that disrupts the electrochemical gradient. Cellular tonicity is also disturbed, causing lethal transmembrane fluid shifts. If these changes do not cause immediate cell death, they often initiate apoptosis. The ability to visualize ice ball formation, the edge of which marks the 0°C isotherm, in cryoablation on several imaging modalities is a particular benefit.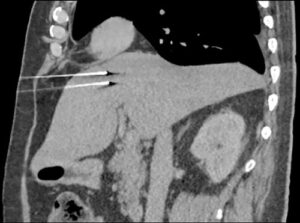 IRE is a nonthermal ablation technique that induces cell death by disrupting the electric potential gradient across cell membranes, leading to the formation of permanent nanopores through the plasma membrane, altering cellular transport and ultimately cell homeostasis.5 The procedure involves the delivery of a series of high voltage direct current electrical pulses between two electrodes placed within a target area surrounding the tumor. Since IRE is a nonthermal treatment, it has the advantage over thermal ablative treatments since the treatment zone can cross large blood vessels and bile ducts without damaging these vital structures.
IRE is a nonthermal ablation technique that induces cell death by disrupting the electric potential gradient across cell membranes, leading to the formation of permanent nanopores through the plasma membrane, altering cellular transport and ultimately cell homeostasis.5 The procedure involves the delivery of a series of high voltage direct current electrical pulses between two electrodes placed within a target area surrounding the tumor. Since IRE is a nonthermal treatment, it has the advantage over thermal ablative treatments since the treatment zone can cross large blood vessels and bile ducts without damaging these vital structures.
 The therapy provides a local tumor treatment which does not block the blood supply to healthy liver tissue.
The therapy provides a local tumor treatment which does not block the blood supply to healthy liver tissue.